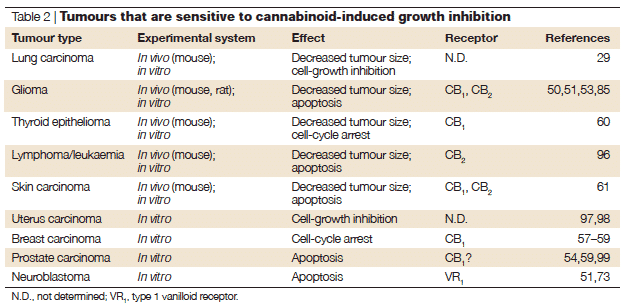
Cannabinoids may provide anti-tumor effects by various mechanisms, including induction of apoptosis, inhibition of cell growth, anti-angiogenic effects and inhibition of production of circulating tumor cells. Cannabinoids appear to kill tumor cells but do not affect their healthy counterparts and may even protect them from cell death. For example, these compounds have been shown to induce apoptosis in glioma cells in culture and induce regression of glioma tumors in mice and rats, while they protect normal glial cells of astroglial and oligodendroglial lineages from apoptosis mediated by the CB1 receptor.
Cancer Statistics:
Daniel E. Ford, M.D., M.P.H.
H.T. Vu, C. Hauer, K.L. Helzlsouer, J.C. Anthony
Johns Hopkins University School of Medicine
Dr. Ford is Associate Professor of Medicine, Epidemiology and Health Policy and Management at the Johns Hopkins University School of Medicine. He graduated from Cornell University and received his medical degree from the State University of New York, Buffalo, completed his residency in internal medicine at Johns Hopkins, and received a masterÕs of public health degree at the same institution. After 2 years of postgraduate training at the National Institute of Mental Health, Dr. Ford rejoined the faculty at Johns Hopkins. For more than a decade he has been a member of the team conducting research on the relationship between psychiatric disorders and physical health in the Baltimore Epidemiologic Catchment area study. Dr. Ford has completed several studies related to tobacco smoking cessation and currently is funded by the National Cancer Institute to develop an Internet-based smoking cessation program. He directs a fellowship program in primary care health services, has published more than 60 articles and book chapters, and is currently Associate Editor for the Journal of General Internal Medicine.
Marijuana smoke contains carcinogens. Several small case series and one potentially flawed small case-control study have provided evidence that marijuana is associated with head and neck cancer. We conducted a large case-control study to address this issue. We recruited 164 participants with consecutive incident cases of head, neck, or lung cancer (adults younger than 55 years) in the Baltimore region from four hospitals between 1994 and 1999. Also recruited as controls were 526 individuals (younger than 55 years) from the Baltimore Epidemiologic Catchment Area study based on a random household sample. Cases and controls completed identical assessments of exposures via self-report, direct computer entry. Lifetime and current uses of marijuana, tobacco, and alcohol were assessed with detailed questions of use by 5- to 10-year intervals of their lives, by weekend and weekday consumption, and by mode of administration of the substance. Control patients were younger (44 vs. 49 years, p<.001), more likely to be female (62 percent vs. 34 percent, p<.001), and less likely to be white (55 percent vs. 69 percent, p<.01). Substance use was commonly reported in both cases and controls (lifetime means, 125,000 tobacco cigarettes, 27,000 alcoholic drinks, and 8,700 marijuana joints). Consistent with other studies, use of tobacco and alcohol was associated with these cancers. Ever use of marijuana (66 percent controls vs. 60 percent cases, p=.17) and lifetime marijuana joints (8,135 vs. 8,946 joints, p=.64) were not associated with cancer. Marijuana use every day for 1 month or longer also was not associated with those cancers, with or without adjustment (19 percent controls, 12 percent cases, odds ratio=.74, 95 percent confidence interval .38, 1.43). Age of first use of marijuana, depth of inhalation of marijuana, and use of pipe versus joint for marijuana were not related to these cancers. Although power was limited, marijuana use was not associated with cancer for those who never used tobacco. Adjusting for all sociodemographic factors, family history of these cancers, lifetime tobacco use, and lifetime alcohol use did not change the relationship between marijuana and cancer. The balance of evidence from this study, the largest case-control study addressing marijuana use and cancer to date, does not favor the idea that marijuana as commonly used in the community is a major causal factor for head, neck, or lung cancer in young adults.
Note: Click here for a reference list of journal articles on Cannabis and Cancer compiled by Dr. Robert Melamede
©2024 MEDICINAL GENOMICS CORPS
Copyright all right reserved.
Signup to receive email updates on blog posts, podcasts, webinars, new products, and more!
Join us at the CannMed 24 Innovation and Investment Summit, an exclusive experience of discovery, development, and networking with innovators from around the world.